Medical school seniors scored a record number of available first-year slots in this year’s Main Residency Match, with both internal medicine and family medicine programs offering more spots to residents in 2016.
Continuing a 4-year growth trend, the number of available post-graduate year 1 (PGY-1) positions rose to 27,860 in 2016, 567 more spots than in 2015, and a record 18,668 U.S. allopathic medical school seniors registered for the match, 221 more than in 2015, according to data from the National Resident Matching Program (NRMP).
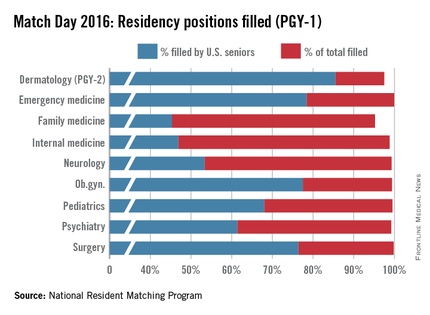
Family medicine residency programs offered 3,238 positions in 2016, up from 3,195 in the 2015 match. This year, greater than 95% of those positions were filled; 45% were filled by U.S. medical school graduates, the NRMP announced March 18.
Internal medicine experienced similar increases, with residency programs offering 7,024 positions this year, up from 6,770 positions in 2015. Just less than 99% of the positions were filled, with 47% filled by U.S. medical school graduates in this year’s Match.
“We’re very pleased with the way the numbers turned out,” said Dr. Philip A. Masters, clinical content development director for the American College of Physicians (ACP). “About 45% of new slots in this year’s Match were in internal medicine. So that coupled with a very high fill rate really suggests a continuing and an increased interest in the field.”
Dr. Wanda Filer, president of the American Academy of Family Physicians, said she was glad to see an increased number of medical school graduates matching to family medicine, but she stressed that the numbers are not enough.
“This nation needs far more family medicine physicians than the current numbers are achieving,” she said in an interview. “The growth in family medicine residency slots is not fast enough and our antiquated graduate medical education payment is misaligned with U.S. workforce needs. Additionally, poor accountability for federal dollars by some U.S. medical schools to deliver that workforce should be rapidly addressed.”
While ACP officials were satisfied with the overall internal medicine numbers, Dr. Masters said that the lack of medical students entering general internal medicine and primary care careers is concerning.
“The number of people in the regular categorical [internal medicine] training programs is a lot lower than it used to be,” Dr. Masters said in a interview. “A long time ago, upwards of half of people who went in categorical training pursued a career in general internal medicine. [Now], the overall trend tends to be away from primary care/general internal medicine. That is concerning because that’s what society really needs right now.”
Pediatric positions, meanwhile, rose slightly in 2016, growing to 2,689, with 21 more slots than last year. Just more than 99% were filled, and 68% were filled by U.S. seniors.
The NRMP data shows that of 18,668 U.S. allopathic seniors who registered for the Match this year, 18,187 submitted program choices and 17,057 matched to first-year positions. This is up from the 18,025 U.S. allopathic medical school seniors who submitted program preferences for the 2015 Match, of which 16,932 matched to first-year positions.
The larger scope of this year’s Match is likely attributed to growing enrollment among medical colleges, said NRMP President and CEO Mona Signer.
“Every year seems to be larger than the year before, at least, certainly recently,” Ms. Signer said in an interview. “It isn’t just a little bit larger. It’s a lot larger. Medical schools have been increasing enrollment and new medical schools have been [opened]. We certainly expect to see that trickle into the Match as those new schools begin to graduate their first classes and as those existing schools begin to graduate larger classes.”
But Ms. Signer agrees with others that larger Match numbers will not necessarily curb future physician shortages.
“The increasing enrollment in medical schools can’t help but at least address the physician-to-population ratio,” she said. “The issue is, are those new physicians gong to be in the specialties that we need? Obviously, we need more primary care physicians. It remains to be seen whether larger class sizes are going to result in a better physician-to-population ratio in primary care.”
On Twitter @legal_med